Let’s talk heel pain, this is a common complaint I see in the clinic. There can be many causes of heel pain. It is important to accurately diagnose heel pain and distinguish the vast causes of heel pain for the appropriate management. Below, is an Algorithm of heel pain from a paper that highlights the complexity around heel pain (see photo underneath of complexity of heel pain).
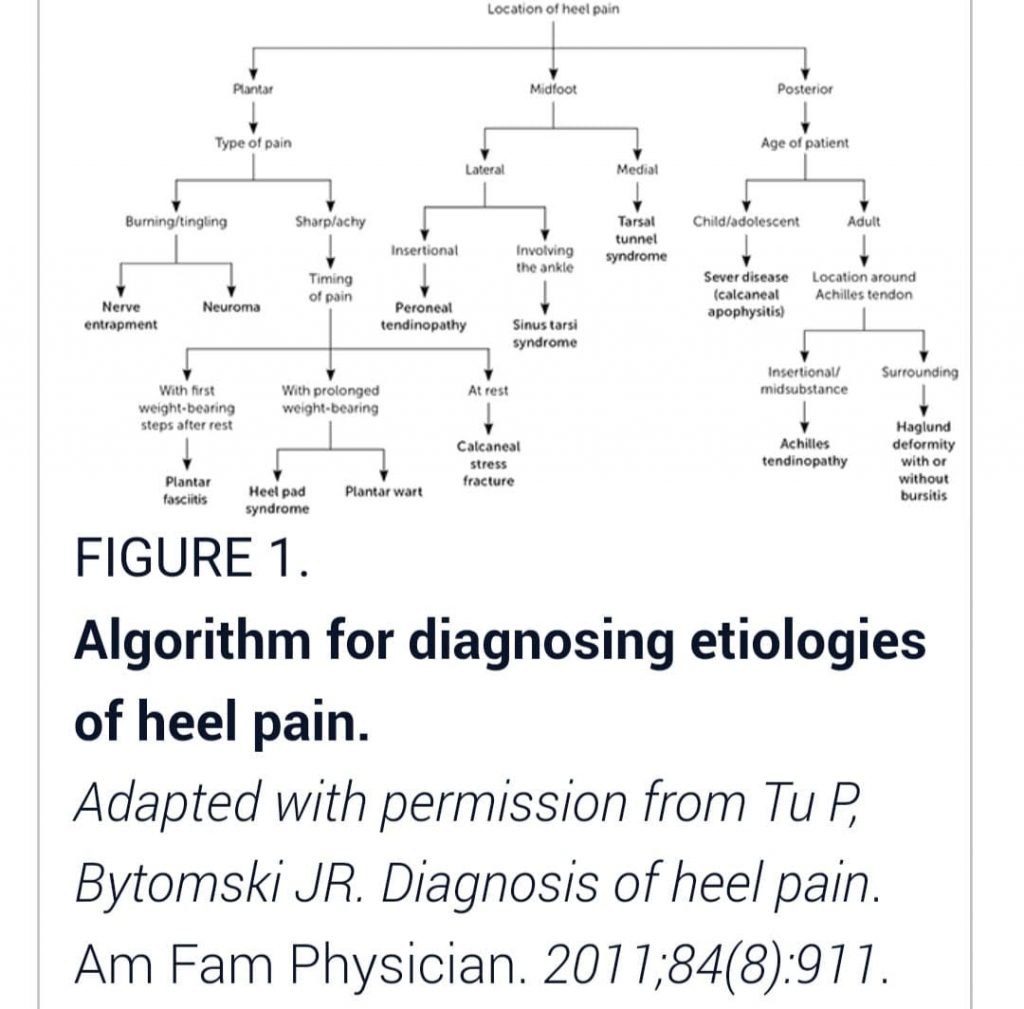
However, for the purpose of this blog, I will concentrate on two of the most common causes of heel pain I see which is plantar fasciosopathy and nerve entrapments.
Plantar fasciopathy
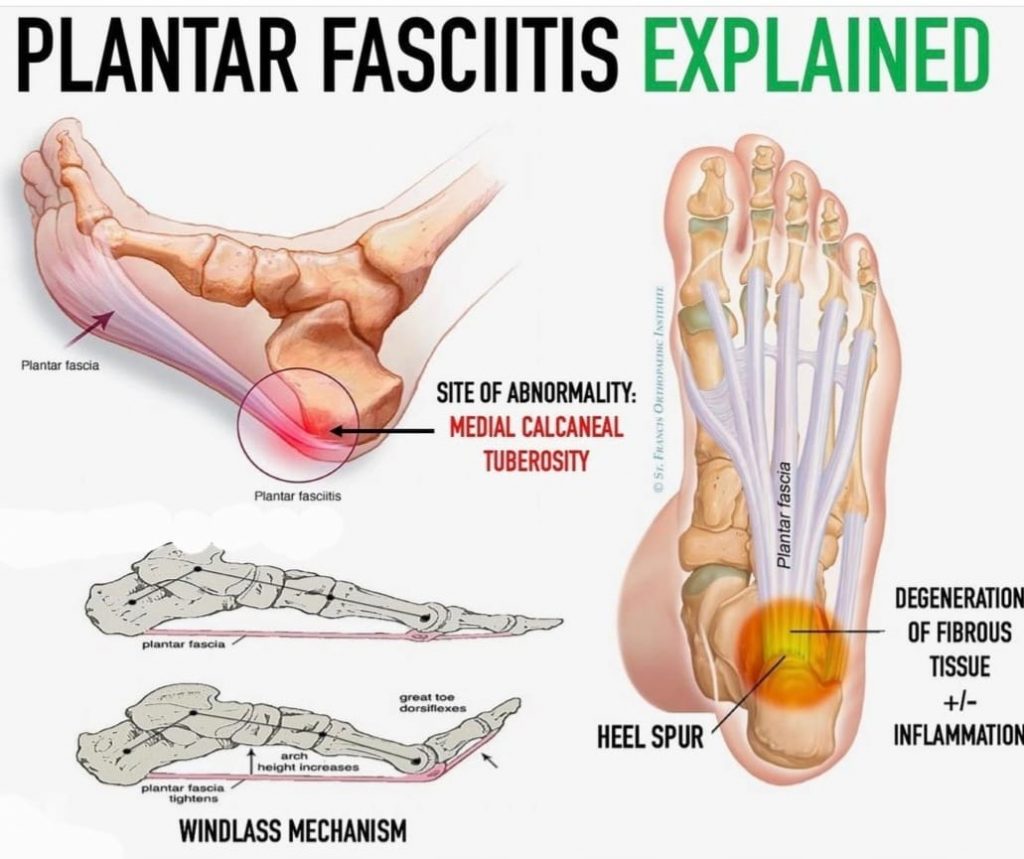
Plantar fasciopathy or plantar fasciitis as it is commonly referred to is the most common cause of heel pain in the adult population. The plantar fascia plays an important role in foot biomechanics.
How does the plantar fascia act during walking?
- It stiffens the arch and reduces the arch from flattening
- It helps resupinate the foot for propulsion
- Reduces ground reaction forces
- Helps absorb and release energy during running
What is the windlass mechanism?
Tension is placed on the plantar fascia which causes compression of the midfoot, raising the arch which creates mid-foot stability for effective propulsion (see photo plantar fasciitis explained above)
It is generally an over use injury where micro tears develop in the plantar fascia, followed by secondary degeneration.
Risk factors
It usually multifactorial condition with interrelated risk factors associated in its development from one person to another.
- Advancing age due to age related changes to the tissues within the fascia which decrease its ability to resist tensile loads
- Overuse due to prolonged weightbearing
- A higher BMI increases tensile forces on plantar fascia and can rupture
- Flat feet
- Poor foot biomechanics which lead to mechanical overload and degeneration of the plantar fascia
- Training errors, such as a sudden increase in activity or not enough time in between loading of activities
- Reduction of either both or one of ankle dorsiflexion range of motion and 1st MTPJ range of motion may increase strain loads on the plantar fascia
- Occupation, may be standing on hard surfaces all day
Symptoms
Typically, pain is around the medial aspect of the plantar heel and is aggravated with first steps in the morning or after periods of rest, which routinely gets better during the day and then resurfaces again at rest (show photo of plantar fascia anatomy).
Management
- Stretching on the Achilles muscles take tension off the plantar fascia.
- Strengthening exercises provided may reduce strain on the plantar fascia and strengthen the arch of the foot.
- Kensiology Taping- Initially, to provide support, lessen pain, decrease swelling and improve function.
- Low level laser therapy – is often used in the acute and chronic cases of heel pain whereby it reduces inflammation, reduces pain and promotes healing of the soft tissues in the surrounding tissues and the site of pain.
- Prolotherapy – A 5% dextrose solution injected into or around the site of pain. Sometimes, accompanied with local anaesthetic nerve block
- Custom foot orthoses- Can be used to aid inarch support and offload painful areas
- Shockwave therapy is commonly used for the more chronic heel pain individuals
- Footwear- Arocker bottom shoe may provide comfort when walking, allow for a more efficient gait and may reduce pain
Nerve entrapments
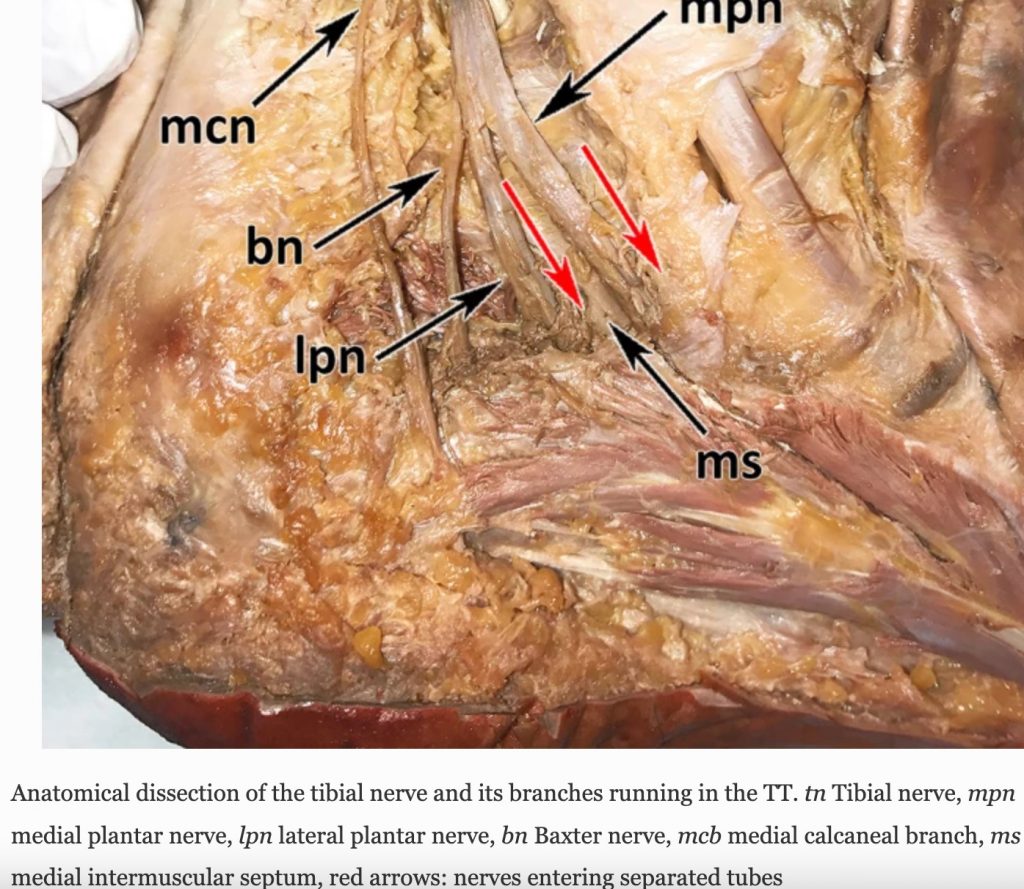
Arguably, the second most common cause of heel pain I see in the clinic would be nerve entrapments. I will briefly discuss a few nerve entrapment types I see in the clinic. (To the right have photo of nerves from cadaver)
Tarsal tunnel syndrome – is an entrapment of the tibial nerve under the flexor retinaculum on the medial side of the ankle. Generally due an anatomical variation, structural anomoly putting pressure on the nerve- eg ganglion cyst, varicosties, abductor hallucis muscle, fascia irritation. Patients generally have pain, tingling, numbness basically along the whole bottom of the foot.
Medial calcaneal neuropathy – Medial calcaneal nerve is a branch of the posterior tibial nerve which carries sensory information from the skin over the plantar surface of the calcaneus and subcutaneous fat and part of the forefoot. It’a entrapment is likely caused from a tight plantar fascia, or other structural variations – ganglion sacs, varicosities etc. Patients often complain of a burning pain, pins and needles around the skin of the calcaneus and into part of the forefoot. See nerve anatomy below, and the sensory mapping of individual nerves categorised by the coloured regions.
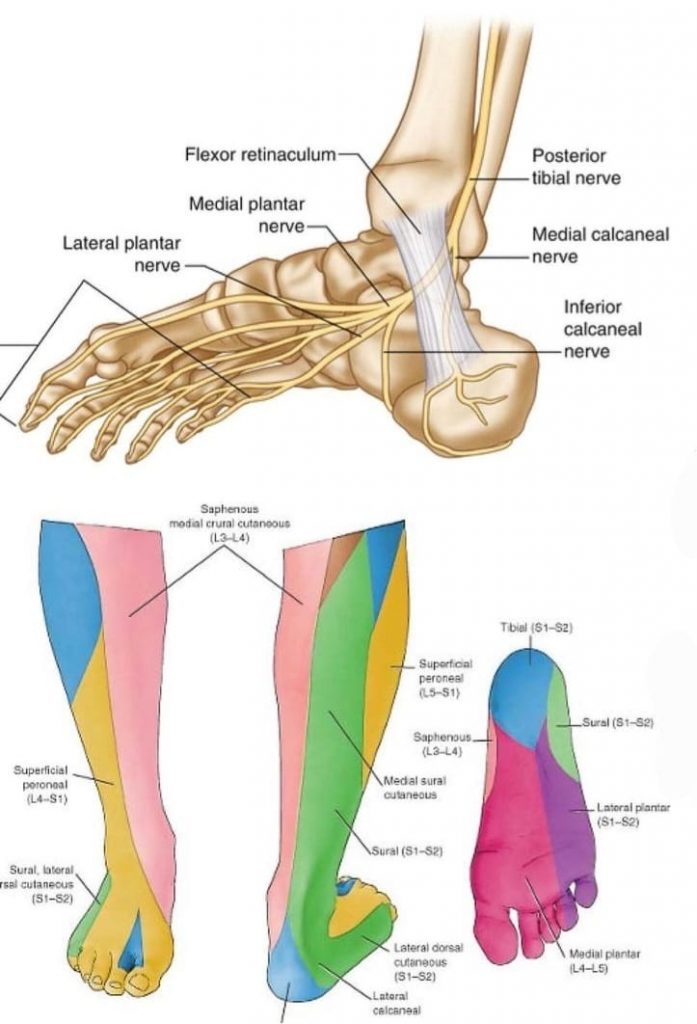
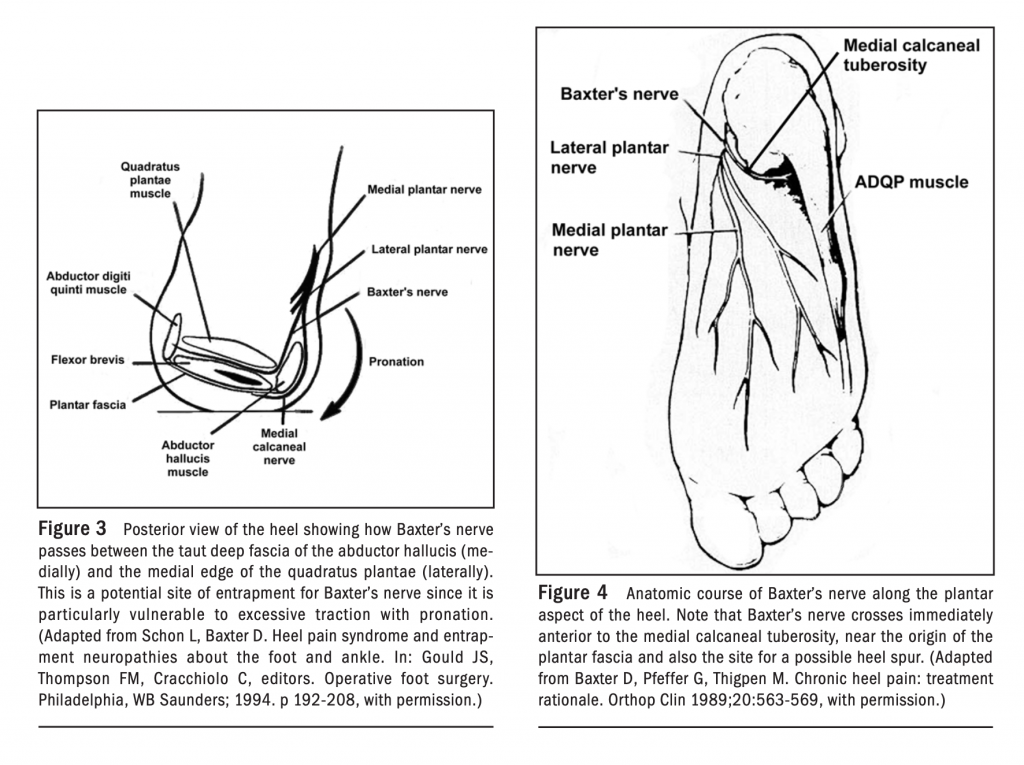
Baxter’s nerve – is the first branch of the lateral plantar nerve. It supplies motor innervation to the quadrates plantae, flexor digitorum brevis, and abductor digits minima muscles within the foot, in addition, it provides sensory information from the calcaneal periosteum and long plantar ligament. It primarily gets entrapped distally between the abductor hallucis and the quadrates plantae muscles or in the calcaneal tuberosity between flexor digitorum breves and quadrates plantae muscles. Patients often describe a sharp, radiating pain along the course of the lateral plantar nerve (Baxter’s nerve). Pain is often brought on by walking and at times night. (see below baxter’s nerve anatomy)
Management
- Low level laser therapy – is a good option for nerve related heel pain as it reduces the inflammation around the nerves which is causing the pain and promotes healing of the tissues surrounding the area
- Prolotherapy – A 5% dextrose solution injected into or around the site of pain. Sometimes, accompanied with local anaesthetic nerve block
- hydrodissection– High volume injections of various injectants-5% dextrose, or anaesthetic mixed with saline. This technique relieves the pressure on the entrapped nerve and freeing it from any surrounding tissues, resolving the nerve symptoms.
- Custom foot orthoses- Can be used in some cases, with a shock absorbing cover and redistribute plantar pressures away from the site of pain
Moroni, S., Zwierzina, M., Starke, V. et al. Clinical-anatomic mapping of the tarsal tunnel with regard to Baxter’s neuropathy in recalcitrant heel pain syndrome: part I. Surg Radiol Anat 41, 29–41 (2019). https://doi.org/10.1007/s00276-018-2124-z
Latest News
Ankle Arthritis
Understanding Ankle Arthritis and Regenerative Treatment Options in Podiatry Ankle[…]